In this blog , we are going to discuss about causes, symptoms and treatments
What Is Ascites?
Ascites can be defined as a medical condition that entails the accumulation of excessive fluid in the peritoneal cavity, which is located between the abdomen lining and adjacent abdominal organs.
Therefore, it produces major protuberance in the stomach hence some people call it different names such as peritonitis, hydroperitoneum, and so forth. It is not a standalone disease but rather a manifestation of many underlying health problems in humans which may be severe.
- For instance, the existence of fluid within the peritoneal space can signify conditions such as liver diseases, cancer, cardiac failure, or even infections. Thus proper diagnosis and management are the key since the underlying causes will greatly influence prognosis and also treatment approaches.
Causes, Symptoms, and Treatments:
Gross Appearance of Ascites Fluid:
The ailments and understanding that ascites diagnosis as well as understanding ascites diagnosis from a clinical standpoint rely on the gross appearance of the fluid. This fluid can inform us significant information about the underlying problem that has led to its accumulation.
Color of Fluid:
1) Translucent Or Yellow:
This is often a sterile or normal fluid. The occurrence of a translucent or yellowish shade indicates that the fluid might have low infectivity and/or contamination. This can be observed in cases where the ascites are not associated with an infection but due to cirrhosis of the liver.
2) Brown:
A brownish coloration is connected with hyperbilirubinemia. Hyperbilirubinemia describes a situation where there is more than enough bilirubin in blood which in turn can be linked to conditions of the liver and also blockage of bile ducts.
3) Bilirubin:
Bilirubin, which results from normal breakdown of red blood cells, could get deposited in the liquid found within the cavity in case it accumulates owing to liver’s incapacity for the treatment process.
4) Cloudy Or Turbid:
Evidence of infection is usually shown by turbid or cloudy fluid. The white blood cells, bacteria or other inflammatory cells are the reasons for the frequently cloudy fluid. In other words, the body has an inflammatory reaction against a pathogen which could be one of the following: bacteria, viruses or fungi.

On paracentesis, the ascitic fluid appeared milky and turbid.
5) Pink Or Blood-Tinged:
There may be pinkish or blood-tinged fluids in mildly traumatized cases. It occurs when there is slight bleeding into the abdomen which is likely to be from a recent injury or through any surgical procedure done that damaged blood vessels present.
6) Grossly Bloody:
If there is grossly bloody fluid this indicates malignancy chances exist. Blood-stained ascitic fluid indicates the spread of cancer particularly abdominal and gastric cancers to the peritoneum lining or other abdominal organs.
Causes of Ascites:
The development of ascites can be attributed to several underlying causes, each of which includes complex physiological processes. To do accurate diagnostics and prescribe treatment, it is crucial to comprehend these factors.
- Schistosomiasis: The leading cause of ascites is liver fibrosis cirrhosis. In this process, the liver tissue becomes scarred, making it incapable of functioning correctly. As the liver continues to degenerate due to the accumulation of scar tissue, blood vessels supplying the liver become pressurized, resulting in portal hypertension; this condition causes fluid leakages from blood vessels into the peritoneal cavity, producing ascites.
- Liver Cancer: Hepatocellular carcinoma refers to the classiest type of liver cancer development which also causes ascites accumulation. The allowing for obstruction of tumors within the liver increases both blood flow resistance thus making portal hypertension worse along with fluid gain.
Liver disease is the most common cause of ascites
- Hepatitis: Chronic hepatitis, especially Hep B & C virus attack over time may lead to a decline in the efficiency with which the liver processes and filters out toxic substances from the bloodstream thereby causing it to lose its ability to perform these vital functions efficiently. Unfortunately for patients suffering from cirrhosis, damage done to the hepatic cells due to inflammation puts them at further risk for developing ascitic fluid collecting in their peritoneal cavity.
- Ovarian Cancer: Ascites among women can be notably caused by ovarian cancer. The cancerous cells may spread onto the peritoneal lining thereby causing irritation and increased production of fluids. On top of that cancer cells can block lymphatic vessels thereby preventing normal drainage of peritoneal fluid.
Ovarian Cancer and Ascites: A Hidden Connection
- Intestinal Cancer: Ascites can be an outcome of both small as well as large intestinal cancers particularly when the cancer cells invade the peritoneum or cause bowel obstruction which may lead to fluid collection within the abdominal cavity.
- Heart Failure: When the heart cannot pump enough blood around the body, it fails (known as congestive heart failure – CHF). The result is that the veins that carry blood away from these organs do not drain properly; there is always some backflow depending on how much time elapses between heartbeats.
- In this way, CHF causes blood vessels of the liver to become congested and leads to increased intra-hepatic pressure at its best moments, causing fluids to collapse into the peritoneal cavity termed ascites.
- Pancreatic Conditions: Diseases of the pancreas such as pancreatitis or pancreatic cancer cause ascites too. Inflammatory processes or malignancies within the pancreas could irritate the peritoneum or cause obstruction of lymphatic drainage which results in the accumulation of fluids.
- Viral diseases: Some airborne viral diseases like influenza cause whole-body inflammation and retaining of fluids which contribute to the formation of ascites especially if there are existing diseases in the person.
- Alcoholism: One of the key risk factors for cirrhosis of the liver is chronic intake of alcoholic drinks which is also one of the principal causes of ascites. On account of alcoholic damage to liver cells, the organ becomes incapable of regulating its work properly and redistributing fluids.
- Abdominal or Intestinal Tuberculosis (ATB/ITB): Tuberculosis may affect the abdomen and intestines resulting in a condition known as peritoneal tuberculosis that causes prominent inflammation within the peritoneal lining leading to accumulation of ascitic fluid.
Signs And Symptoms of Ascites:
Although the development of ascites shows remarkable differences which can be attributed to the amount of fluid and etiology involved, there is little change in external appearance at first. Sometimes in the early days, there may be no symptoms without a rate of development that is high enough to trigger them.
Common Signs And Symptoms Include:
- Abdominal Swelling and Pain: Ascites in their early stages do not have any noticeable symptoms, especially if the amount of fluid that is collected is too small. When the fluid in the peritoneal cavity increases, it causes visible swelling of the abdomen (Organs around it do ache because they are under pressure). The abdomen could be tense or distended.
- Sudden Weight Gain: Rapid weight gain without cause is a common indication for ascites. Most of the time, this comes about because there has been some build-up of water rather than increased body fat or muscle mass (the more water in your system, the more your weight). The additional weight that comes with fluid may be huge.
- Swollen Ankles: If one has peripheral edema, then it is probable that ascites are present mostly in the legs or ankles. This happens because whenever a person retains some amount of fluid in the belly section of their body; it will distribute itself around different areas.
- Increased Waist Size: When the abdomen inflates the waist expands. Due to that clothes may be close fit such that they may not be wearable anymore like belts or waistbands which used to fit well.
- Fatigue: A general sense of weariness or lack of energy accompanies individuals with asceticism. The body works harder to keep from having too much water inside it as well as causing discomfort resulting from starvation-related illness.
- Heartburn and Indigestion: Increased pressure on the stomach as a consequence of enlarging the abdomen can result in heartburn (pyrosis), gastroesophageal reflux disease (GERD), or indigestion (dyspepsia). For this reason, much food intake worsens these symptoms.
Gastroesophageal reflux disease (GERD), also known as acid reflux or heartburn, is a chronic digestive disease.
- Constipation: When there is a build-up of ascitic fluids pressing onto the intestines, they tend to become constipated or have bad bowel habits. This reduces the movement of waste through one’s intestines, preventing them from passing stools normally
- Nausea and vomiting: Ascitic patients may occasionally experience nausea and vomiting. For example, they might undergo such symptoms because of stomach or intestinal pressure and also any problems linked with the liver or gastrointestinal tract that cause fluid retention itself.
Grading System For Ascites:
Ascites are commonly categorized based on their severity, allowing for informed results on treatment and displaying how fast or slow the disease progresses. The grading system for ascites can be divided into three groups:
Grade 1: Mild Ascites:
- When it arises to grade 1 ascites, it can be categorized as an accumulative collection of insignificant-sized fluid that is observed only via ultrasound or CT. An inexperienced doctor may not even realize there isn’t much happening in the patient’s body. Most frequently this type of liquid lies at either the hepatorenal angle or some other pockets within the abdominal cavity.
Grade 2: Moderate Ascites:
- Moderate amounts of free fluid characterize grade 2 ascites in the peritoneal cavity. It results in a more pronounced uniform expansion of the abdomen. Intestines may become displaced due to fluid collection around them; they could also appear floating in imaging studies.
- More visible signs are noted on patient’s body with some developing symptoms related to increased abdominal pressure. experience symptoms related to the increased abdominal pressure.
Grade 3: Large Ascites:
- In grade 3 ascites, a substantial quantity of fluid builds up in the abdominal cavity that causes noticeable swelling or distention. This makes the belly feel tight and very painful. The navel may push outwards as a result of the tension.
Prevention And Control Of Ascites:
Ascites, often a result of liver disease, heart failure, or other medical issues lead to the build-up of fluid in the abdomen. A combination of lifestyle changes and medical interventions are needed for managing and preventing it. Below are key strategies for the prevention and control of ascites:
- Limit salt intake: Cutting back on salt consumption averts water retention and stomach swelling related to ascites.
- Maintain a healthy weight: Overweight status can lead to the worsening of pre-existing conditions such as liver disease hence management of weight is paramount.
- Increase albumin intake: One should increase the amount of protein food they eat to boost albumin levels which helps avoid excess water in tissues.
- Avoid sugar and unhealthy fats: A diet high in sugar and saturated fats can worsen liver diseases and cause a patient’s fluid retention. Instead, focus on whole grains, fruits and vegetables.
- Regular medical check-ups: Regular checking up ensures that treatment is adjusted in good time whenever there is an occurrence of ascitic fluid accumulation.
- Abdominal ultrasound: In the early stages of fluid build-up, this imaging method can be utilized for averting intervention.
- Avoid smoking: Smoking harms both the blood vessels and organs by raising susceptibility to conditions that can lead to ascites.
- No alcohol: Overindulgence in alcohol can harm the liver, hence causing ascites. It is essential to restrict alcohol consumption.
- Regular exercise: This will help keep your weight within recommended limits through proper circulation thus reducing fluid accumulation risks.
- Limit fluid intake: As per your doctor’s recommendation use less amount of fluids in order not to make things worse than they are now in terms of water retention.
Sonographic Features Of Ascites:
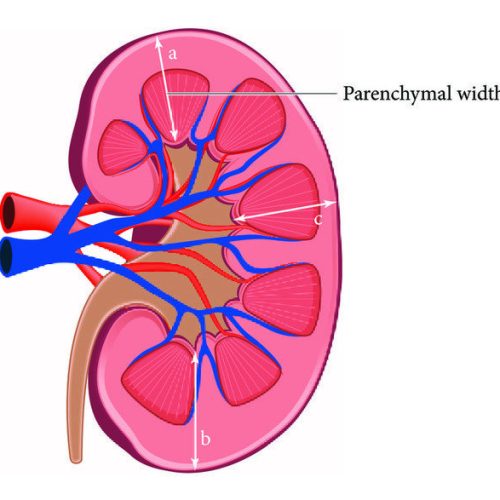
The peritoneal cavity, normally empty of liquid, is the space lying between the abdominal lining and the abdominal organs in a healthy person. During an echo graphic examination, the absence of expression in this cavity is a normal finding.
- When effusion occurs, though, this space begins to get filled with fluid, whose first signs can be detected by sonography.
The earliest detectable fluid accumulation due to effusion is usually found in abdominal recesses like the hepatorenal angle or Morrison’s pouch which is located between the liver and the right kidney. Even as little as ten milliliters of fluid can be characterized from this area using high-resolution ultrasound.
The image above organizes an example of how ascites will appear on abdominal ultrasound
- This makes it possible for ultrasound to assist in the early diagnosis of effusion even before it becomes apparent by clinical observation.
In the presence of fluids, they are often echo-free or anechoic on the ultrasound screen meaning that they don’t produce any sound echoes inside them hence appearing like dark or black spots on the image created by ultrasound; this happens because pure liquids (for example serous fluid) do not reflect sound waves to a transducer of ultrasound.
Nevertheless, peritoneal effusions are not all neat or devoid of other fluids. Blood, pus, or other particulate matter may sometimes blend in with the effusion. This condition may give rise to internal echoes which are seen on ultrasound images. Such internal echoes appear as spots or more solid areas scattered throughout echogenic liquid. Investigating these internal echoes can reveal very valuable information concerning ascites’ origin.
For example, seeing them indicates hemorrhagic ascites (containing blood), infected ascites (containing pus including inflammatory debris) or chylous ascites (containing lymphatic fluid with fat).
Therefore, it can be said that ultrasonographic characteristics of ascites comprise the detection of any fluid in the places where there is no hepatorenal angle and its ultrasound presentation without any echo. Internal echoes found within the fluid may indicate that this form of ascites has been complicated by blood, pus, or other components.
Treatment of Ascites:
The management and treatment of ascites depend on the underlying cause and also how serious it is. Paracentesis, which mainly involves fluid removal from the peritoneal cavity, is one of the main treatments for ascites.
- Since it entails both sampling for diagnosis and relieving symptoms resulting from fluid accumulation, this procedure can be termed as diagnostic and therapeutic.
Before paracentesis can be approved, fasting may be necessary. This helps to reduce the risk of complications during the procedure such as nausea or vomiting, which can happen if someone has an empty stomach.
- It also helps ensure that bowel movements are not full when undergoing this procedure so as not to perforate bowels.
In paracentesis, the patient is positioned in a way that allows fluid to pool in one area of the abdomen for easy access. Generally, ultrasound guidance is used in conducting paracentesis so that doctors can pinpoint the precise location of the fluid and avoid damaging nearby organs or structures.
- The thickness of the abdominal wall, its depth, and how thick or thin is the liquid are particularly determined through ultrasound technology. For needle size selection depending on these measures as well as entry point selection will be so important because they all matter.
- After identifying the best area to administer the injection, the doctor cleans it with an antiseptic solution to minimize the chances of infection. A local anesthetic is then injected under the skin and deeper tissues to numb that part of the body where needles are going to be inserted.
After compartment is numb, a needle fixed to a thin tubing called cannula is passed through the abdominal wall into the peritoneal cavity carefully. The needle punctures a thin membrane surrounding the abdomen called the peritoneum through which fluid can be reached.
- Once this done, through the cannula, a collection bag will be filled with the draining fluid. Depending on how much fluid there is and how sick a patient is, one may need different amounts safely discharged. Sometimes only little bits may come out for purposes of diagnosis alone; however in other instances, more than enough volumes are siphoned off to ease conditions like stomach ache or even breathing difficulties.
The doctor will continuously observe the patient’s vital signs and rate of draining fluids throughout the process. If too much liquid is removed from one’s body blood pressure can decrease dramatically or electrolytes might go haywire; hence such processes must always take place slowly and carefully.
At last after draining all unwanted substances this needle-cannula setup is removed together with its insertion site cleaned up using sterile dressing.
In certain instances, the liquid could be dispatched to a laboratory where it will undergo analysis. Through this analysis, the primary cause of abundant fluid in the peritoneal cavity like infections, cancers, or liver ailments can be recognized. This information obtained from the fluid analysis helps to direct succeeding treatment which may involve changes in diet, medicine, or procedures.
- Paracentesis is a safe procedure in most cases although, like other medical interventions, it comes with some risks.
These risks include but are not limited to; bleeding, infection, internal organ injury, and rarely post-paracentesis circulatory dysfunction which occurs when body fluids shift thus causing low blood pressure and kidney failure. Paracentesis should only be done by an experienced health provider under sterile conditions with monitoring measures put in place.
To conclude
Treating ascites usually involves paracentesis-a surgical technique used to remove additional fluid from the peritoneal cavity. During this process, ultrasound is applied so as to ensure that removal of these fluids is done safely while minimizing complications at the same time. Additionally, paracentesis not only relieves symptoms but also plays a substantial role in identifying its underlying causes thus making more focused and active treatment possible.