Learn about the causes, symptoms, diagnosis & treatment of urinary tract infections, including uncomplicated and complicated UTIs, recurrent infections & more.
Urinary Tract Infections:
presence of microorganisms in the Urinary Tract Infections that cannot be accounted for by contamination. The organisms have the potential to invade the tissues of the urinary tract and adjacent structures.
Definitions:
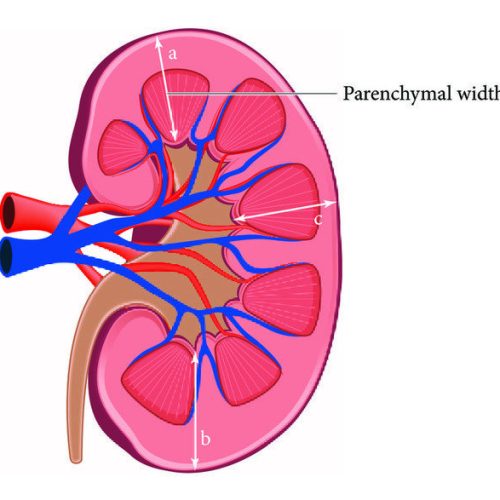
- Anatomic
- Lower: Urethritis, cystitis (superficial infection of bladder), epididymitis, prostatitis.
- Upper: Pyelonephritis (inflammatory process of the renal parenchyma), renal or perinephric abscess Clinical.
- Uncomplicated: Cystitis in immunocompetent nonpregnant women w/o underlying structural or neurologic disease.
- Complicated UTIs: Upper tract infection in women or any UTI in men or pregnant women or UTI with underlying structural disease or immunosuppression.
- Uncomplicated UTIs: are not associated with structural or neurologic abnormalities that may interfere with the normal flow of urine or the voiding mechanism.
- Complicated UTIs: are the result of a predisposing lesion of the urinary tract, such as a congenital abnormality or distortion of the urinary tract, stone, indwelling catheter, prostatic hypertrophy, obstruction, or neurologic deficit that interferes with the normal flow of urine and urinary tract defenses.
- Recurrent UTIs:, two or more UTIs occurring within 6 months or three or more within 1 year
Get more Information.
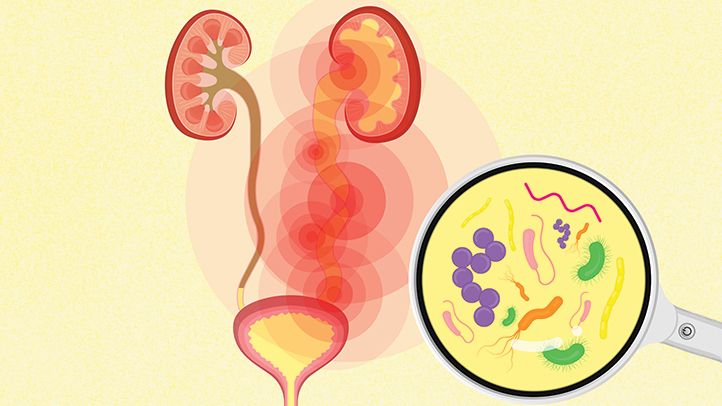
Microbiology:
- Uncomplicated UTI: E. coli (80%), Proteus, Klebsiella, S. saprophyticus, Pseudomonas aeruginosa, and Enterococcus spp.
- Complicated UTI: E. coli (30%), enterococci (20%), Pseudomonas (20%), S. epidermidis (15%), Proteus spp., K. pneumoniae, Enterobacter spp other GNR.
- Catheter-associated UTI: yeast (30%), E. coli (25%), other GNR, enterococci, S. epi.
- Urethritis: Chlamydia trachomatis, Neisseria gonorrhoeae, Ureaplasma urealyticum, Trichomonas vaginalis, Mycoplasma genitalium, HSV.
- S. aureus: uncommon primary urinary pathogen in absence of catheter or recent instrumentation; consider bacteremia w/ hematogenous seeding in patients with stones, indwelling urinary catheters, or chronic renal abscesses, multiple organisms may be isolated.
Clinical Presentation:
- Cystitis: Dysuria, urgency, frequency, hematuria, ( in urine color/odor, suprapubic pain; fever generally absent.
- Urethritis: May be identical to cystitis except urethral discharge may be present
- Prostatitis
- Chronic: Similar to cystitis except symptoms of obstruction (hesitancy, weak stream)
- Acute: Perineal pain, fever, tenderness on prostate exam.
- Pyelonephritis: Fever, shaking chills, flank or back pain, nausea, vomiting, diarrhea.
- Renal Abscess (Intrarenal or Perinephric): Identical to pyelonephritis except persistent fever despite appropriate antibiotics. Elderly patients will present with altered mental status, change in eating habits, or gastrointestinal (GI) symptoms.
Diagnostic Studies:
- Urinalysis: Pyuria, bacteriuria & hematuria & nitrites
- Urine Cx show significant bacterial counts: “105 CFU/mL in asx women, “103 CFU/mL in men, “102 CFU/mL in sx or catheterized Pts (hydration may falsely dilute counts) pyuria & ! UCx * sterile pyuria S urethritis, nephritis, renal tuberculosis, foreign body
- Pregnant women & those undergoing urologic surgery: screen for asx bacteriuria
- Blood cultures: in febrile and possibly complicated UTIs
- DNA detection/cx for C. trachomatis/N. gonorrhoeae in high-risk Pts or sterile pyuria
- 1st-void and midstream urine specimens, prostatic expressage, and post–prostatic massage urine specimens in cases of suspected prostatitis
- Abdominal CT to r/o abscess in Pts with pyelo who fail to defervesce after 72 h
- Urologic workup (renal U/S w/ PVR, abd CT, voiding cystography) if recurrent UTIs in men
- The nitrite test can be used to detect the presence of nitrate-reducing bacteria in the urine (eg, E. coli).
- The leukocyte esterase test is a rapid dipstick test to detect pyuria.
- The most reliable method of diagnosing UTIs is by quantitative urine culture. Patients with infection usually have more than 105 bacteria/mL [108 /L] of urine, although as many as one third of women with symptomatic infection have less than 105 bacteria/mL [108 /L].
Treatment:
- Cystitis: FQ or TMP-SMX PO + 3 d (uncomp.) or + 10–14 d (complicated) Asx bacteriuria in pregnancy or prior to urologic surgery S abx + 3 d
- Catheterized Pts: Abx as above and remove or exchange catheter Urethritis: Treat for both Neisseria and Chlamydia
- Neisseria: ceftriaxone 125 mg IM + 1
- Chlamydia: doxy 100 mg PO bid + 7 d or azithromycin 1 g PO + 1
- Prostatitis: FQ or TMP-SMX PO + 14–28 d (acute) or 6–12 wks (chronic) Pyelonephritis
- Outpatient: FQ or oral ceph. PO + 14 d
- Inpatient: ceftriaxone IV or FQ PO or aminoglycoside or ampicillin/sulbactam + 14 d (( IV S PO when Pt improved clinically and afebrile + 24–48 h and then complete 14-d course)
- Renal Abscess: Drainage ! antibiotics as for pyelonephriti.
Treatment And Symptoms Of UTI?
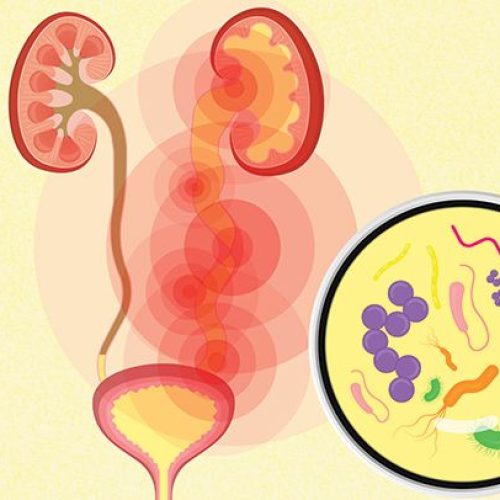
It can involve any part of your urinary system. Bacteria especially E. coli are the most common cause of UTIs. Symptoms include needing to pee often, pain while peeing and pain in your side or lower back. Antibiotics can treat most UTIs.
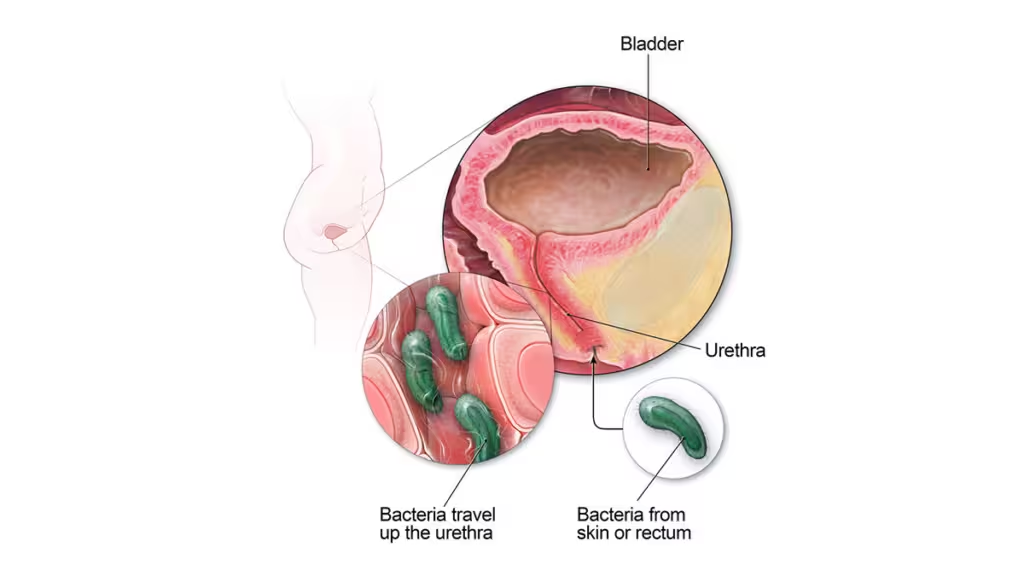
Main Cause Of Urinary Tract Infection?
UTI s typically occur when bacteria enter the urinary tract through the urethra and begin to spread in the bladder. The urinary system is designed to keep out bacteria. But the defenses sometimes fail. When that happens, bacteria may take hold and grow into a full-blown infection in the urinary tract.
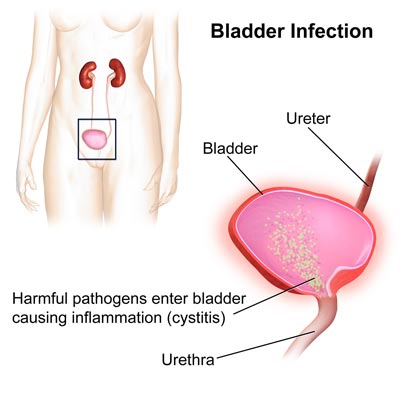
5 Warning Signs Of Bladder Infection?
Symptoms of lower UTI Include:
- Feeling a strong urge to urinate (pee) and more often than usual, a constant, dull pain in the pubic region and pain when urinating (dysuria)
- Cloudy urine (pee) or blood in your urine (haematuria)
- Urine that smells unusually unpleasant.
- Back pain.
- A general sense of feeling unwell.
Can I Treat Urine Infection Myself?
If you have a mild UTI, it might go away on its own over a few days. If you’re not pregnant or at higher risk of developing a complication from a UTI, you may be able to hold off on antibiotics for a couple of days to see what happens. Get medical care if your symptoms don’t start to improve after a couple of days.
What Is The Fastest Way To Treat UTI?
It’s standard for a doctor to prescribe antibiotics for UTI treatment. After starting antibiotics therapy, symptoms usually improve within 2–4 days . Many doctors prescribe an antibiotic for at least 3 days. If the UTIs don’t clear up after antibiotic therapy, it may mean that you need a different type of antibiotic.